In the global race to curb the pandemic, scientists are testing a new kind of vaccine. Roger Highfield, Science Director, talks to key figures in the ‘David and Goliath’ race for a COVID-19 ‘RNA vaccine’.
A protective vaccine is the most effective way to end the pandemic and, of the 160 under development around the world, a new kind is being tried in Britain, Germany, China, and the United States.
Known as an RNA vaccine, it turns cells in the body into vaccine factories and, once it is shown to work, it can be made quickly and in large amounts.
One RNA vaccine is under test by Robin Shattock of Imperial College London is backed by £41 million in funding from the UK government, notably from the UKRI-Medical Research Council, and a further £5 million in philanthropic donations.
Tal Zaks is the Chief Medical Officer of the US company Moderna and its RNA vaccine candidate is backed by $483 million from the US Biomedical Advanced Research and Development Authority (BARDA), along with billions of investment, with more than $1 billion of private capital raised this year alone.
Moderna, which specialises in developing therapies based on messenger RNA, became the first company to test a vaccine against SARS-CoV-2 in humans when it launched a trial in March.
Their responses, distinguished by RS (Robin Shattock)and TZ (Tal Zaks), are shown below in italics.
Update, November 16: Moderna announced that a study of its RNA vaccine candidate against COVID-19 in more than 30,000 participants achieved an efficacy of 94.5%. “This positive interim analysis from our Phase 3 study has given us the first clinical validation that our vaccine can prevent COVID-19 disease, including severe disease,” said Stéphane Bancel, Chief Executive Officer.
Update, December 8: Margaret Keenan, 90, becomes the first person in the world to be given the Pfizer-BioNTech RNA vaccine as part of a mass vaccination programme in the UK.
Update, January 8 2021: Moderna’s RNA COVID-19 vaccine approved by the Medicines and Healthcare products Regulatory Agency.
HOW CONFIDENT ARE YOU THAT ONE OF THE 160 VACCINES WILL WORK?
RS: Although vaccine success rates tend to be around 10 per cent at the clinical testing stage, I am optimistic that several effective vaccines will emerge.
I have told the House of Lords Science and Technology Committee that the chance of finding an effective vaccine is high.
But it’s not just a matter of rushing out the first wave of vaccination – we also need strategies to maintain immunity, for instance with a booster vaccination, if that’s required.
WHAT IS RNA?
In living things, the genetic information that contains the instructions to make protein building blocks of cells is carried in the form of the long chain-like chemicals, RNA, and DNA (ribonucleic acid and deoxyribonucleic acid, respectively.)
Thirty years ago, it was shown that the direct injection of nucleic acids (RNA or DNA) into the muscles of mice led to them making the proteins encoded by the injected nucleic acid.
In the case of RNA, molecular machines, called ribosomes, use the RNA to turn genes into flesh and blood: a so-called messenger RNA molecule carries the instructions for making a protein from the cell’s storehouse of genetic information, held in the form of DNA.
To turn this messenger RNA code into a protein, the ribosome harnesses a second type of RNA – transfer RNA – which carries the building blocks of proteins, called amino acids, to assemble a protein.
WHAT IS AN RNA VACCINE?
Many traditional vaccines are based on a weakened or modified form of virus, or parts of it, but the Imperial and Moderna vaccines are based on synthetic strands of genetic code (RNA), using part of the virus’s genetic material.
TZ: What our vaccine does, unlike any other, is teach the body’s own cells to make that little bit of the virus that the immune system of the body needs to recognise.
So, if you’re walking down the street and somebody with COVID-19 sneezes on you, your immune system goes ‘Well, hang on a second. I’ve seen that before’ and it can mount an immune response so that you don’t get sick.
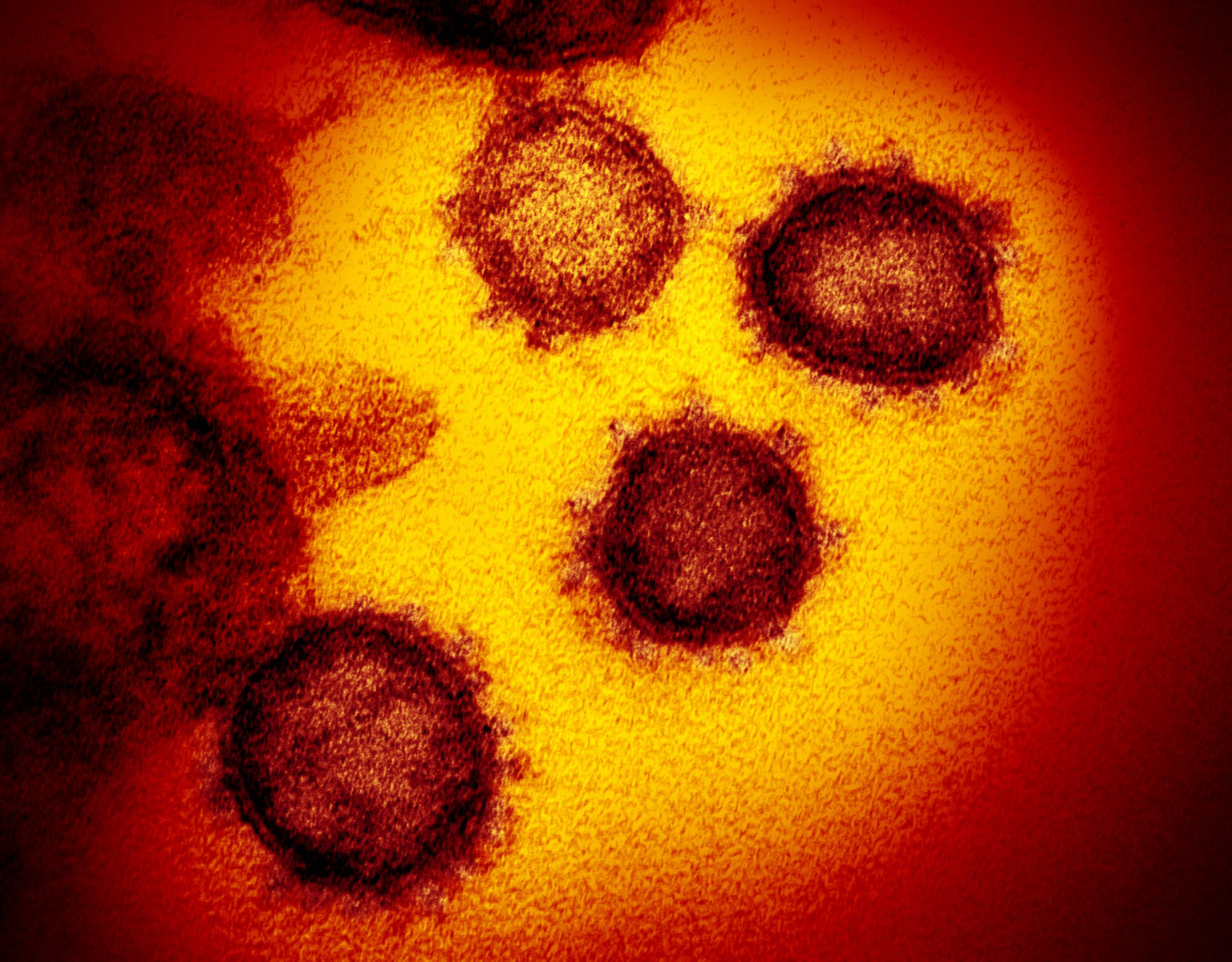
When it comes to Moderna, we don’t start with the virus and try to make inactivated or attenuated versions of it, but instead just take the genetic information that encodes for that piece of the virus that the immune system sees, which is the spike protein that’s on the surface of the virus.
We basically just take that information and encode it in a transient manner in a way that allows the body’s own cells to make it. So we injected that information – in the form of the genetic code RNA – into the muscle, and then it goes into your immune system where the cells in the immune system pick it up and they start making this protein.
And as they make it, they kind of look at it and say ‘hold on, I’ve never seen that thing before.’
That revs up the immune system and you start to make antibodies, which are proteins that attach and block foreign bits of microbes and viruses that shouldn’t be there. In this way, we can educate the immune system in a very specific manner.
RS: At Imperial, we have also taken the code for the surface ‘spike’ protein that gives the virus its crown-like appearance (“corona” is crown in Latin) for which it is named, and made our genetic vaccine.
There is nothing of the virus in there, just RNA genetic code for one part of the virus. The RNA goes inside fat droplets, is injected into muscle, where it instructs them to make the spike protein which, we hope, tricks the immune system to think it has seen the whole virus.
HOW LONG HAVE YOU BEEN WORKING ON AN RNA VACCINE?
TZ: We started the clinical research a little over five years ago, also against a pandemic threat, a strain of flu that people were worried would come out of China at that time. Over the past five years, we’ve been improving the science and applying it to more vaccines.
We have been quite successful in revving up the immune system to recognise different parts of different pathogens.
Up until the end of last year, the most advanced vaccine was against cytomegalovirus, an infection that women sometimes transmit to their babies before they are born, which is the number one cause of neurological birth defects.
HOW ABOUT MODERNA’S PANDEMIC VACCINE?
TZ: We had a meeting on September 29 of last year with Tony Fauci (the best-known member of the Trump Administration’s White House Coronavirus Task Force) to talk about what could be a demonstration project for this technology, taking a randomly selected virus, starting the stopwatch and see how fast you can go to a vaccine.
Lo and behold by December we started to hear about this new respiratory virus and in January the genetic sequence of the virus was known and we said: ‘This isn’t a drill. This is a live fire.’
We’ve taken this vaccine into the clinic in collaboration with the US National Institutes of Health.
We’ve shown already in phase one, the first trial of our COVID RNA vaccine in humans, that we do get to very significant levels of these blocking or neutralising antibodies. So, we believe we are showing the body the right part of the pathogen to raise an immune response.
We’re on track to start a very large trial this month (phase three trial) that aims to show if we can not only generate an immune response but prevent disease.
HOW LONG DID IT TAKE IMPERIAL TO MAKE ITS RNA VACCINE?
RS: In 2018, at a presentation at the World Economic Forum, I said there’s going to be another pandemic.
We need a technology that can respond quickly, and our self-amplifying RNA technology is one way to do this. Back then, we were expecting avian influenza, but it turned out to be coronavirus.
We downloaded the sequence of the coronavirus when it was released by Chinese scientists in January and made a template for our RNA-based vaccine in two weeks. The normal cycle for developing a vaccine is two years.
HOW CONFIDENT ARE YOU THAT RNA VACCINES WILL WORK?
RS: What we are doing is both state of the art and simple.
I’m cautiously optimistic this approach will work as well as anything else being developed because it induces good immune responses in animal models.
We predict it will be the same in humans and it will be very safe because we are using such low doses.
What we don’t know is what level of immunity is required to prevent infection with SARS-CoV-2.
If all goes well, we are hopeful a viable vaccine could be available as early as Spring 2021.
ARE YOU SURE THE SPIKE PROTEIN IS THE BEST TARGET FOR THE VACCINE?
TZ: We’re as confident as science can make us without having proven the point with a phase three trial.
SARS-CoV-2 has close cousins, SARS and MERS. They all share some form of this membranous spike protein, which is the hook that the viruses use to attach to human cells. If you can direct the immune system’s attention to this hook and block the hook, then it stands to reason that the virus can’t adhere to cells.
We’ve studied the ability of vaccines against this spike protein to block SARS and MERS in animal experiments all the way up through camels and non-human primates.
Some of these other viruses have demonstrated that, indeed, with just immunity against the spike protein you can prevent infection and disease of those cousins of SARS.
If you can generate those neutralising antibodies against the spike, you can also prevent infection and in some cases disease in those animals so it is as good as it’s going to get until we conclusively show in humans that indeed, vaccinating with this vaccine prevents disease.
WHAT ARE THE ADVANTAGES OF RNA VACCINES?
They offer a way to make a vaccine at pandemic speed – all that is required is the genetic sequence of the virus causing the pandemic.
RS: This technology is enormous because you can make so much relatively quickly. Our self-amplifying RNA technology means a large amount of vaccine doses can be made in manufacturing facilities with a small footprint.
In a one litre volume, we can make two million doses of a vaccine. To make that same amount with a conventional approach, you might need 10,000 litres.
They can be mass-produced cost-effectively on a large scale. We do need a cold chain – likely 2-8C in the first instance.
Later we may bring our a freeze-dried formulation that can be stored at room temperature that does not require uninterrupted cold storage – that cold chain makes vaccines challenging to distribute in poor countries and rural areas with unreliable refrigeration.
TZ: As far as scaling up, we started months ago. Now the challenge here is that it’s a novel technology nobody’s ever scaled it up to this level. We’re confident that for the same fundamental technical reasons that we’ve been able to start so fast, we should be able to scale up fast.
We expect to have 100 million doses or so by the end of this year, and up to a billion in 2021. Not enough to serve the entire planet, but certainly a sizable chunk.
WHY DO YOU HAVE TO PUT YOUR RNA VACCINE IN FAT PARTICLES?
RS: The main thing in the body that destroys RNA are enzymes called RNases that just chew it up. And they’re everywhere, your skin, saliva, whatever because you do not want foreign RNA hanging about. So, if you exclude those enzymes, your RNA is much more stable.
We call it a fat droplet, so people can understand it, but in fact, it is protected in a specialised structure called a lipid nanoparticle, of the order of a few billionths of a metre in size, similar to the coronavirus particle.
(There used to be great interest in using fat particles called liposomes, notably developed by Alex Bangham, which could deliver drugs through the fatty membrane of cells, and you can think of these lipid nanoparticles as a liposome with a bag of little liposomes that have the RNA.)
We inject these lipid nanoparticles into muscle cells where they start making the spike protein. The RNA probably also gets into immune cells that are attracted to the muscle.
TZ: Think about it from an evolutionary perspective.
RNA is basically an instruction template, foreign to the cell, that’s coming in to tell the cell what protein to make. There is nothing scarier to either a unicellular organism or a multicellular organism like you and me than a foreign bit of messenger RNA trying to instruct your body what to do.
Evolution has evolved countless mechanisms both at the single-cell level and at the organism level to counteract that. In our early years of research, we’ve had to devise methods to overcome that.
What we do is engineer this lipid nanoparticle around the RNA so that in the body it actually looks like a little fat blob and so it doesn’t trip up the immune response to block it as foreign before it even gets into the cell.
When you put the particle into muscle, by and large, it will flow with the lymphatic drainage, the system that presents foreign stuff to our immune system.
Once it gets into the body’s immune cells the RNA escapes from the lipid nanoparticle and, because we manufacture the RNA in a certain way, once it’s inside the cell, it doesn’t look foreign and molecular machines there – ribosomes – turn that RNA into a protein, spike protein from COVID-19 in this case.
HOW DO YOU MAKE SURE YOUR RNA INSTRUCTION IS ACCEPTED BY A CELL?
TZ: SARS-CoV-2, for example, is an RNA virus.
One of the things we’ve learned over time is when a foreign virus comes in and tries to take over cells, when it uses the cell’s own building blocks, the cell is capable of recognising whether one of those building blocks in the wrong place. That in turn triggers one of those innate immune responses to fight the invader.
To overcome this innate response, we put a little naturally occurring modification on that building block and manufacture the messenger RNA in a very particular way so that the evolutionary sensory system is blocked. It, therefore, doesn’t see it as foreign, and so the cell can carry out the instructions.
It took us a while to understand how critical these steps are to generate a potent amount of protein. Once we did that, we could show time and again that indeed we’re successful in our ability to generate vaccines.
The lifetime for the vaccine RNA is 24 to 48 hours, after which the RNA is degraded so it’s just like cell food. One messenger RNA molecule will make thousands of protein copies before it is degraded.
The protein it makes can linger a little bit, to generate an immune response.
WHAT IS DIFFERENT ABOUT THE IMPERIAL WORK?
RS: As Tal Zaks says, when RNA goes into cells it is often seen as foreign, and you make what we call an innate response which involves a signaling protein called interferon.
That innate immune response is why, if you get influenza or COVID-19, you feel cold and shivering.
Moderna have modified their RNA to reduce that response. But compared with us they’re using quite a lot of RNA.
We get past that innate response by using a dose of RNA that is 100 times lower than their dose, not enough to make an individual feel unwell but in the Goldilocks zone. Just enough to make the immune system say, ‘Oh, there’s something going on in the muscle’, to trigger the immune response that will, we hope, protect against coronavirus.
To use a much lower dose, we amplify our RNA vaccine by using enzymes from the Venezuelan Equine Encephalitis Virus. These polymerase enzymes copy the RNA, a bit like a photocopier, to make multiple copies of that initial copy that gets in.
At the same time, they copy the RNA of the target for the vaccine, which is the spike protein.
WHERE IS IMPERIAL’S VACCINE IN TERMS OF TRIALS?
The Imperial vaccine underwent pre-clinical safety tests and in animal studies, it has been shown to be safe and produced encouraging signs of an effective immune response.
On 23 June, the Imperial team gave the first dose of a self-amplifying RNA vaccine to a volunteer, with a second booster dose to follow within four weeks. In this study, the team will look to assess the safety and find the optimal dose of the vaccine as they give gradually larger doses to 15 healthy participants aged 18 to 45.
RS: We are really excited that the vaccine has gone into the first participant. This marks an important step for our vaccine, which has never been trialed in humans.
We’re inundated with people who want to be in the trails and spending much more time dealing with people who are disappointed – either because the trial is full or because they don’t meet the eligibility criteria – than the trial itself.
The Imperial team will recruit another 300 healthy volunteers (aged 18-75) to trial the optimal dose of vaccine. If the vaccine is safe and shows a promising immune response, a trial involving 6,000 people is planned for October.
RS: We need to assess whether the vaccine can train the immune system to defend itself against COVID-19. We eagerly await when we can assess both the safety of the vaccine and its ability to produce neutralising antibodies. The vaccine can then be rolled out to more people in the UK and beyond.
WHEN CAN WE EXPECT THE RESULTS OF MODERNA’S FINAL, PHASE THREE, TRIAL?
TZ: Our best estimate is Moderna’s phase three trial will start this month and is a matter of immunising the right people.
If we take people like me who can sit at home all day long and avoid exposure, nobody’s going to get infected, so we won’t know if the vaccine works.
So, the trick is to vaccinate those people who can’t avoid the risk of infection, such as health care workers. Some proportion of them will, by bad luck, get exposed in the coming months and so we hope to be able to demonstrate that the people who got vaccinated don’t come down with the disease relative to those who didn’t.
We’re going to be counting cases by the end of this year, with some chance even by Thanksgiving. So, by mid-November, we should have enough interim cases to be able to say that this vaccine indeed works.
RS: When we do our big study in the UK in October, in the same way, a big challenge is if we see enough infections quickly enough to be able to compare how the vaccinated group do compared with the placebo.
We are looking to do it somewhere else in the world as well just to get that answer quicker.
WHAT ARE THE RISKS?
TZ: We’ve been thinking about it for years. I do not believe that there’s a theoretic concern that messenger RNA will have a toxicity that manifests when you use it as a vaccine than, say, if you use it as a drug, as others do.
My personal belief is that it’s likely to be safer because you’re able to focus the attention of the immune system just on that thing that you wanted to recognise.
The second component is the lipid nanoparticle, which is new. One lipid component is cholesterol, present in minuscule amounts, and another is a synthetic lipid that we invented that is cleared in hours and we haven’t seen any significant toxicity to date.
The third element is the protein. There is history in the 1960s of using the preservative formalin to inactivate a virus, like a measles virus, and this had a chemical effect on the proteins in the virus, and so it skewed the immune response to cause worse disease rather than preventing disease.
The beauty of RNA vaccines is that we are translating the protein within our own cells using our own ribosomes, so it is physically impossible for ourselves to generate the wrong protein.
There are also worries that you don’t know what you don’t know. Maybe you’re hyper-focusing the immune system, and that’s bad somehow. But all the trials that we’ve done, whether they’re in preclinical models, in animal models or in the initial clinical studies, we’ve seen the typical safety profile of a vaccine.
In the place where you inject our vaccine, it can hurt a little bit, maybe cause some redness, soreness, and swelling. When you’re activating the immune system, you may see some brief flu-like symptoms, a fever, and some headache which, to me, actually is a sign of having some good potent immune activation.
I’d rather have an evening of flu-like symptoms than COVID-19, right?
WILL AN RNA VACCINE WORK AGAINST NEW STRAINS OF COVID-19?
RS: In terms of SARS-CoV-2 mutations, we don’t see evidence that the virus is changing very significantly, which is very reassuring.
Even if it does change, some of the technologies like the one we’re using can easily be adapted to deal with any changes in the virus that might occur in the future.
HOW CAN WE BE SURE EVERYONE CAN BENEFIT FROM THESE VACCINES?
RS: We must think about how to make vaccines not just for the whole of the UK but the whole of the world.
Imperial has formed a social enterprise VacEquity Global Health (VGH), in partnership with Morningside Ventures, to rapidly develop vaccines and distribute them widely, including to low- and middle-income countries.
Imperial and VGH will waive royalties and charge only modest cost-plus prices to sustain their work, accelerate global distribution, and support new research.
TZ: This is an element of success worth double-clicking on. We have to make sure that we collaborate with the right people, notably governments, to ensure that those who need the vaccine the most are those who get it first.
Without a true public-private partnership, no one company can do this.
WHAT OTHER RNA VACCINES ARE UNDER DEVELOPMENT?
Among the other RNA vaccines under development, are:
CureVac, a German-based company, specialising in mRNA vaccines, also using lipid particles, has started clinical trials against Sars-CoV-2.
Preliminary results from a trial of an RNA vaccine by BioNTech and Pfizer – making what is called the SARS-CoV-2 receptor-binding domain (RBD), which binds to receptors on host cells during the process of viral entry. – showed ‘positive data’ in 45 subjects.
They reported only mild to moderate reactions, significantly elevated antibodies, and SARS-CoV-2 neutralising antibodies.
Further data from the ongoing Phase 1/2 clinical trial of four vaccine candidates will enable the selection of a lead candidate and dose level for a global Phase 2b/3 study that may begin soon.
If the safety and efficacy study is successful, and the vaccine receives regulatory approval, the companies are expecting to manufacture millions of doses by the end of 2020 and potentially more than 1.2 billion doses by the end of 2021.
In America, Arcturus Therapeutics, which works on RNA vaccines, and Catalent, which offers advanced manufacturing, are working on LUNAR-COV19 – a low dose, potential single shot COVID-19 vaccine.
In China, CanSino Biologics is working on an mRNA vaccine delivered in lipid nanoparticles with Precision NanoSystems, and the People’s Liberation Army (PLA) Academy of Military Sciences is working on another with Walvax Biotech.
CAN YOU USE MORE THAN ONE VACCINE?
RS: Yes. For example, the Oxford University/Astra Zeneca prototype vaccine (based on a modified virus), which is ahead of the field as the first in large human trials, and the Imperial vaccine could be used together.
If you use two different approaches – one to prime the immune system, then change to another to boost it, you often give you a better response.
WHAT OTHER FACTORS CONCERN YOU?
TZ: We live in a divisive age. Many people have many concerns about vaccines in terms of safety. I think those concerns are legitimate and they come from honest places where people come at this problem from different viewpoints.
It is incumbent upon all of us in this field to listen and understand these concerns.
Ultimately everybody must make a choice for themselves on whether they want to get vaccinated. But we must be willing to take into consideration those concerns so that when the solution is out there, the benefit can be maximised.
RS: The anti-vaccination movement is anti-evidence. With the RNA technology, some people mistakenly think that we’re doing gene therapy, that we’re changing people’s genes.
But RNA is transient and doesn’t affect your chromosomes. That is an information battle we will have to solve. I suspect these vaccines will be safer than any other vaccine.
However if and when we or Moderna or one of the others get a sign the vaccine works, people will want to rush it into mass-producing it rather than studying it for a couple of years to build up the safety data. At that point, we will look like heroes.
Five years down the line, however, when the vaccine’s gone into 10s of millions or hundreds of millions of people, some of them will have adverse responses, or something happens to them that they associate with the vaccine.
Whether it’s caused by the vaccine or not, you can very quickly go from being a hero to a villain.














Comments